MANAGE: Bladder urgency
The Key in the Lock Phenomenon and Urge Incontinence
Ever felt the sudden urge to rush to the toilet as soon as you get home, or when you hear running water? This is often due to what's known as the key in the lock phenomenon — where certain triggers can make you feel like you have to go right away, even if your bladder isn’t that full yet.
In simple terms, it's like your brain’s “bladder control” switch flips when it senses familiar cues — like the sound of a flushing toilet, the feeling of a cold key in the lock, or even just arriving home. These cues can make your bladder muscles contract, causing you to experience a sudden, intense urge to urinate.
For people with urge incontinence, this phenomenon can lead to accidents, because their bladder muscles contract too soon or too strongly before they’ve made it to the toilet. The bladder is ready to release urine even if it’s not yet full, often triggering leakage.
This kind of response is part of an overactive bladder, where the bladder becomes too sensitive to cues, leading to urgency, frequency, and sometimes leakage. But don’t worry, bladder training can help retrain the bladder to recognize these triggers and give you more control.
If you recognize the "key in the lock" effect in yourself, it may be helpful to incorporate strategies like delaying urination for a few minutes when you feel the urge or using relaxation techniques to calm down the bladder’s overactive response.
What Should You Expect from Your Bladder?
What is normal bladder function?
A healthy bladder can hold about 300–400ml of urine during the day and up to 800ml at night. Typically, most people urinate 5–6 times during the day and maybe 1-2x at night, depending on how much they drink.
Normal bladder function means:
- Feeling the need to urinate when your bladder is about half full
- Being able to wait to go to the toilet (without feeling an urgent need or leaking)
- Emptying the bladder completely each time
- Not needing to go too often (no more than every 2–4 hours during the day)
If any part of this process goes awry — like frequent urgency, leakage, or difficulty holding urine — it might signal that something is off. Bladder training or other strategies can help get things back on track.
About Bladder Training
Bladder training is a way to help your bladder get better at holding on — so you don’t feel like you’re always rushing to the toilet or waking up through the night. The goal is to help you feel more in control, with fewer urgent trips and better comfort.
Bladder training can help you:
- Reduce that constant “need to go” feeling
- Learn to wait until your bladder is properly full
- Pass a decent amount of urine each time, instead of small dribbly wee
Bladder Diary
All About the Bladder
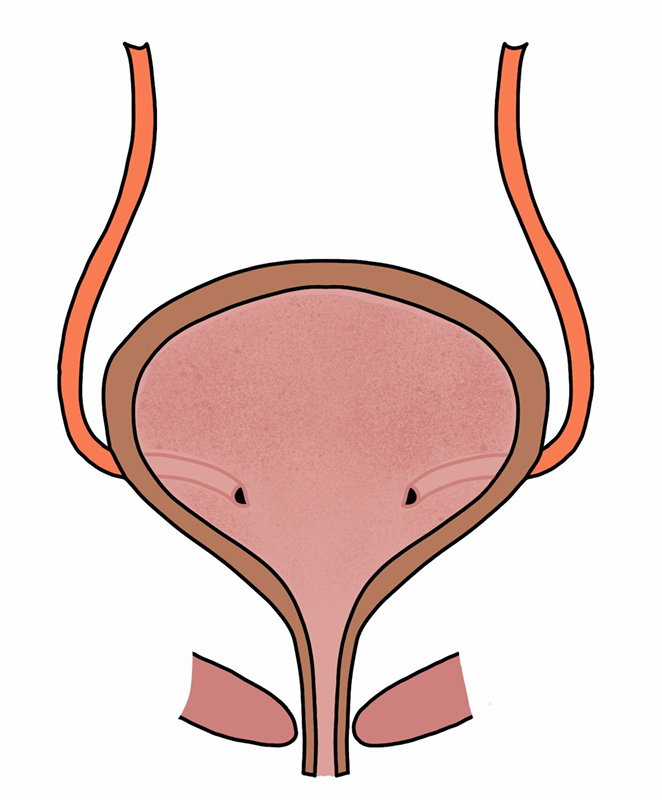
The bladder is a hollow, stretchy organ in your pelvis that holds urine (wee) until you’re ready to empty it. It's connected to your kidneys, where urine is made, and the urethra, which is the tube that lets the urine out when you go to the toilet.
The bladder has a muscle called the detrusor that contracts to push urine out when you go. As it fills with urine, stretch receptors in the bladder wall send signals to your brain, telling you when it's time to go. The sphincter muscles around the urethra stay tight to hold the urine in until you're ready. When you're ready to empty your bladder, these sphincter muscles relax, and the detrusor contracts, sending the urine out through the urethra.
Going to the toilet at night
As we age, we produce less of the hormone (vasopressin) that helps the kidneys concentrate urine overnight — so we make more dilute urine at night. Plus, when we lie down, there's increased blood flow back to the kidneys (venous return), which can also boost urine production. If fluid tends to pool in your legs during the day, elevating your legs in the afternoon can help shift that fluid earlier, so your kidneys deal with it before bedtime.
Drink cups, not sips
Drink a full glass of water at a time rather than sipping throughout the day — this allows your bladder to fill properly, which helps stretch the bladder muscle the way it’s designed to. That gentle distension is important for maintaining healthy bladder function and reducing that constant urge to wee.
Medication: oxybutinin
Oxybutynin is a medication used to calm down an overactive bladder. It works by relaxing the bladder muscle (called the detrusor), so it doesn’t contract as often or as strongly. This can help if you’re experiencing:
- Sudden, strong urges to wee (urgency)
- Going to the toilet frequently
- Bladder leakage (urge incontinence)
By reducing the sensitivity and spasms of the bladder muscle, oxybutynin helps you hold on longer and avoid accidents.
Possible side effects include: Dry mouth (very common), Constipation, Blurred vision, Drowsiness, Sometimes confusion, especially in older adults
These side effects happen because the medication doesn’t just affect the bladder — it also acts on other parts of the body where similar nerves are involved.
Sometimes, a smaller dose of oxybutynin can still help manage bladder symptoms, but with fewer side effects. This can be a good option if you’re sensitive to the typical side effects like dry mouth or constipation but still want some relief from urgency and frequency. Adjusting the dose can help balance effectiveness while avoiding those more uncomfortable reactions.
Another medication option - Solifenacin
What about solifenacin?
Solifenacin is a newer medication in the same family (anticholinergics) but tends to be a bit more targeted, with fewer side effects for many people. It’s often better tolerated, especially if dry mouth or cognitive side effects were a problem with oxybutynin.
It works the same way — calming the bladder muscle and helping reduce urgency, frequency, and leakage.
However, solifenacin is only funded in New Zealand if you’ve tried oxybutynin first and found it didn’t suit you (due to side effects or lack of effectiveness).
A bit of my experience
When I first started using medications like oxybutynin, I thought they’d be a long-term solution. But through bladder training and really understanding how your body responds, I’ve learned that these medications don’t have to be forever. They’re a helpful tool to get you on the right track, but with the right training and habits, you can reduce reliance on them and feel more in control of your bladder without them long term.
Health Library
Learn - Pelvic health