Understanding Menstruation
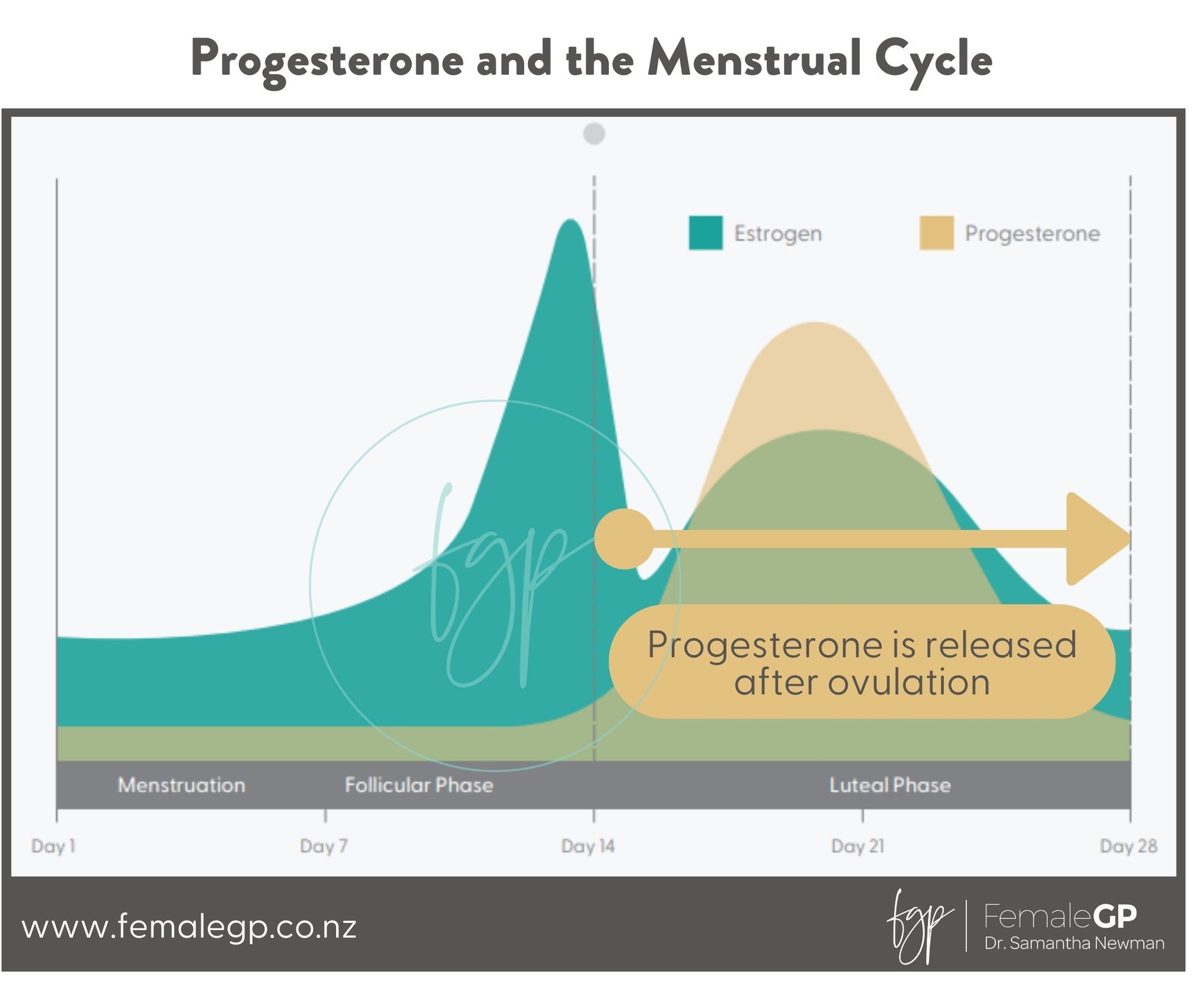
The Menstrual Cycle
Indeed, it is natural, yet we must still strive to learn and comprehend it. While it may be a part of nature, it doesn't imply that it won't occasionally lead to challenges or affect our quality of life. Thus, gaining insight into what is happening is essential for figuring out how to improve our circumstances. It's not merely about enduring difficulties.
Menses management
Menstrual Discs
A menstrual disc offers high capacity, sometimes self-empties, doesn’t rely on suction, works well for those with a lower cervix, and can be worn during intercourse.
Pads
Pads offer versatile period protection, with disposable options in various absorbencies (from light to overnight), winged or wingless designs for comfort and security, and softer, more breathable alternatives like cotton or reusable cloth pads, which are eco-friendly and gentle on the skin.
Menstrual cups
A menstrual cup is a great option because it’s reusable, cost-effective, holds more than a pad or tampon, and can make periods more manageable with fewer changes needed throughout the day.
Abnormal bleeding
What is abnormal bleeding? Often we don't know, because it's always been like that. But fundamentally, if it impacts your life - let's try to make it better