Perimenopause
Perimenopause means the time of life before menopause where there is lots of hormonal flux and brain vulnerability. Traditionally perimenopause was defined as lasting 2-5 years and based on changes in the menstrual cycle (eg length and change of flow). However, for many women the mood changes occur prior to the physical symptoms of menstrual change and hot flushes. Therefore perimenopause can easily last 10-12 years, and begin in the late 30s, with out any medical cause for concern. However, for some women debilitating psychological (eg anxiety) and physical (eg migraine, body pains) can occur in the perimenopause.

About Perimenopause
Learn more through our Insights and Popular Updates
How are you feeling?
Hormones can cause havoc throughout all the body. But if we can put the pieces of the puzzle together - it can avoid unnecessary tests and investigations.
Physical Symptoms
Hot Flushes / Night Sweats
Sudden waves of heat, flushing, sweating, often at night.
Why: Estrogen drop disrupts the brain’s temperature control.
Try: MHT, cooling layers, paced breathing, cognitive behavioural therapy, reduce triggers (alcohol, caffeine).
Joint & Muscle Pain
Aches, stiffness, or soreness, especially in the morning or after rest.
Why: Estrogen supports collagen and reduces inflammation.
Try: Movement, magnesium, anti-inflammatory support, transdermal estrogen.
Fatigue
Persistent tiredness, burnout, feeling “wiped out.”
Why: Hormonal shifts + sleep changes + life load = crash.
Try: Rest cycles, adaptogens, B vitamins, tracking energy patterns.
Migraine
More about migrainesHormonal or stress-triggered headaches.
Why: Estrogen fluctuation affects blood vessels and serotonin.
Try: Magnesium, riboflavin, stable hormone support, hydration.
Itchy Skin
Dry, tingling, or crawling sensations—sometimes with no rash.
Why: Estrogen loss thins and dries the skin, affecting nerve endings. Can be worse premenstrual and during menstruation
Try: Rich moisturizers, antihistamines, topical or vaginal estrogen. (NB antihistamines can be drying!)
Constipation
Sluggish digestion, bloating, straining.
Why: Hormones affect gut motility and hydration. Can be worse premenstrual due to rising progesterone.
Try: Magnesium, fiber, water, nervous system regulation.
RED FLAGS: Do not assume it's hormones, and change in bowel habits please seek medical attention
Recurrent Injuries
(e.g. Frozen Shoulder, Plantar Fasciitis)
Chronic or slow-healing tendon and fascia pain.
Why: Lower estrogen weakens connective tissue repair. Changing and low hormones can also exacerbate the pain response (compounded with sleep disturbance)
Try: Soft tissue therapy, fascial care, MHT, testosterone, reduce strain, protein intake, vitamin D, resistance training, yoga
Emotional/Cognitive Symptoms
Irritability & Mood Swings
Feeling easily annoyed, tearful, or emotionally volatile.
Why: Estrogen and progesterone impact GABA and serotonin.
Try: Cycle awareness, CBT, breathwork, nervous system support, MHT.
Low Libido
Less interest in sex, less arousal or response.
Why: Hormonal changes + stress + relational/emotional load.
Try: Testosterone, intimacy work, pelvic care, removing shame.
“I Feel Like I Have ADHD”
More on ADHD and HormonesDistractibility, emotional reactivity, impulsiveness.
Why: Estrogen influences dopamine and executive function.
Try: Structure, time blocking, cycle syncing, explore formal assessment if needed.
Menopause can mimic or worsen ADHD symptoms, but for many, things settle with support—looking at your history can help clarify whether it’s lifelong ADHD, hormonal shifts, or both, and guide the best next step.
Brain Fog
Feeling “off,” slow thinking, forgetting words.
Why: Estrogen impacts memory, focus, and clarity via the hippocampus.
Try: Sleep, hydration, decluttering your load, MHT, self-compassion.
Memory Lapses
Losing words, forgetting steps or tasks.
Why: Sleep + stress + estrogen = temporary disruption, not dementia.
Try: Normalize it, reduce multitasking, brain-supportive nutrition.
Memory lapses are common in menopause due to hormonal changes affecting brain function—far more common than early-onset Alzheimer’s, which is rare and typically linked to family history; try supportive strategies first, but seek medical or neurological advice if concerns persist.
Tingling in Fingers (Paresthesia)
Pins and needles, numbness, or crawling sensations.
Why: Hormonal changes affect nerve conduction and circulation.
Try: Check posture, magnesium, B12, manage blood sugar and stress.
Genitourinary Syndrome of the Menopause
Vaginal Dryness
Vaginal estrogen creamDryness, irritation, or burning in the vagina. Painful sex.
Why: Less estrogen = thinner, less lubricated tissue. This also leads to change in bacteria and decrease in tissue sizes.
Try: Local vaginal estrogen cream (the gold standard!!), organic lubricants, moisturizers. Other options - pelvic physiotherapy, sex(!), DHEA cream
Dr Sam states "everyone should be offered vaginal estrogen cream"
Painful Sex (Dyspareunia)
Discomfort or pain with penetration or touch.
Why: Vaginal atrophy, dryness, pelvic tension.
Try: Pelvic physio, local estrogen, communication, trauma-informed care.
Painful sex is NOT ok! Lots can be done about it.
Urinary incontinence
More about bladder urgencyLeaking urine with coughing, urgency, or movement.
Why: Pelvic floor weakening + tissue thinning from estrogen drop.
Try: Pelvic floor physio, bladder training, vaginal estrogen.
Physical Symptoms
Tinnitus
Ringing, buzzing, or whooshing in the ears.
Why: Estrogen and progesterone may affect inner ear blood flow and nerve signaling.
Try: Stress reduction, magnesium, hearing check, explore hormonal support.
Dry eyes
Stinging, gritty, or irritated eyes, sometimes with blurred vision.
Why: Estrogen helps regulate tear production and eye surface moisture.
Try: Omega-3s, lubricating eye drops, screen breaks, consider HRT if persistent.
Allergies & Histamine Sensitivity
More on ADHD and HormonesNew or worsened allergies, itching, sensitivities.
Why: Estrogen modulates histamine release and clearance. Progesterone is also a mast cell stabiliser, hence can improve hormone stability.
Try: Antihistamines, avoid triggers, stabilize hormones.
Itchy ears
Persistent itchiness in or around the ear canal.
Why: Estrogen drop can dry out delicate skin and increase histamine sensitivity.
Try: Gentle moisturizers, antihistamines, avoid irritants like earbuds or perfumed products, support hormone balance.
Hair loss
Increased shedding or thinning, especially around the crown or temples.
Why: Lower estrogen and progesterone, combined with unmasked androgen sensitivity, can shift hair growth cycles.
Try: Iron and ferritin check, protein intake, scalp massage, minoxidil, hormonal support if needed.
FAQs about Perimenopause
-
How does FemaleGP support patients in perimenopause?
-
Am I in perimenopause?
Finding out if someone is in perimenopause can be challenging. As we specialise in female hormonal and mental health from a GP perspective we are always on the look out for perimenopause. However, at the same time we do not assume symptoms are hormone related. This is why we have longer appointments, with longer time behind the scenes for our clinicians to thoroughly review your previous health journey.
-
Do you prescribe body-identical hormones?
Our preference is to prescribe pharmaceutical grade, licensed, body-identical hormones. For most women on HRT this consists of an estradiol topical patch, with utrogestan (micronized progesterone). However, we provide personalised care, and synthetic hormones can be the best options for some cases. We do not offer compounded hormones, due to variabilities in consistently and uncertainty with safety profiles.
-
Do you prescribe testosterone?
We do prescribe testosterone. However, a consultation for a ‘testosterone prescription’ from our point of view is not as simple as that. We will review your history, current medications, your symptoms and your goals as well as considerations of affordability, risks vs benefit and applicability. Testosterone isn’t licensed, but like all medications we want to make sure we are doing the best for our patients. And in cases where it is appropriate, we are happy to support medications that are off licence.
-
I am in perimenopause but I don’t want HRT. Can you help me?
HRT is only part of our management plans and your wishes are our priority. There are lots of ways to support hormones and wellbeing without medications – both hormonal and non-hormonal. Through sharing your story we will be able to figure out the best ways forward for your health.
-
My symptoms are due to hormones, but HRT hasn’t helped? Can you help?
Absolutely we can try! We can’t promise, but many of the individuals we work with have improvement in wellbeing through our clinic without hormonal medications, or we may use hormonal medications in slightly different ways, or approaches.
-
Is my menopause is bad enough for HRT?
This is a really personal question and requires an individual assessment, but fundamentally, at FemaleGP we will not judge your symptoms and tell you whether your symptoms are bad enough for intervention. We will explore your current symptoms, your experience now, and the options available to improve your quality of life. We also review your past medical history and experience of different stages of hormonal changes throughout life. This is because we believe it gives clues as to how to make an individualised plan to maximise wellbeing in midlife. HRT are one option that can improve menopause symptoms. It is also really important to ensure that other causes of decreased well being are excluded.
-
Why do I have irregular periods?
There are many reasons for irregular periods, but irregular periods can be a sign of your hormones not performing as they should. The causes are also different at different stages of life. It is important to understand the cause of irregular periods. To do this we need to know your previous history, and current symptoms. We often do bloods tests as well.
-
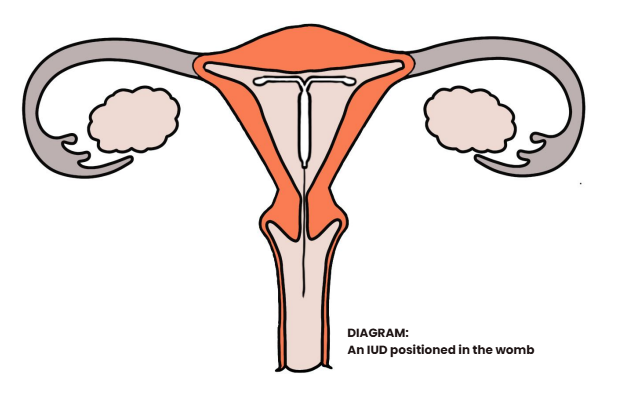
I think I am in menopause but I don’t have any periods because I had a Mirena. Can I do anything to improve my mood?
Absolutely! If you are over 45 years of age, then we don’t need to confirm a diagnosis of menopause. If you are under 45 years of age I like to ensure I’m not missing premature ovarian insufficiency (as we manage that slightly differently). There are lots of support options available, and the Mirena can be part of that!
-
I have had breast cancer. Can you help me with my menopause?
Yes. Life after breast cancer can be a challenge. Some women find that they lose their sense of sense of self, and become defined their new diagnosis. Breast cancer management can also involve medication which triggers ‘menopause’ to help prevent cancer recurrence, or women may have had their HRT stopped.
Management of menopause after breast cancer is really personal. We are happy to talk through the changes one can experience, lifestyle, non-hormonal and hormonal options to improve physical and psychological symptoms of menopause.
-
My periods are really heavy. Is there anything that can be done?
Heavy periods is a common experience in women, particularly at puberty and in perimenopause. At FemaleGP we look into WHY your periods may be heavy, as well as ensuring we improve the flow too. There are many different medications (hormonal, non-hormonal, and intrauterine devices) available, and we also talk about sanitary products. We also talk about tampons and menstrual cups as ways to help improve your quality of life. Iron deficiency can make someone feel tired, have low mood, appetite changes, and ringing in your ears. We take iron deficiency seriously! We also find it really important to explore other possible causes of low iron, and not just assume it is due to menstrual loss.
A course all about Perimenopause
All About Us
The Innovative Online Education Programme to Learn about Hormones and Health
Our Inaugural Course - Perimenopause
Understand your symptoms and general wellbeing to understand where wellbeing can be improved
Button
Lesson 1 - Introduction
Introduction - here we set the scene and explain what lies ahead so you can get the most out of your time
Button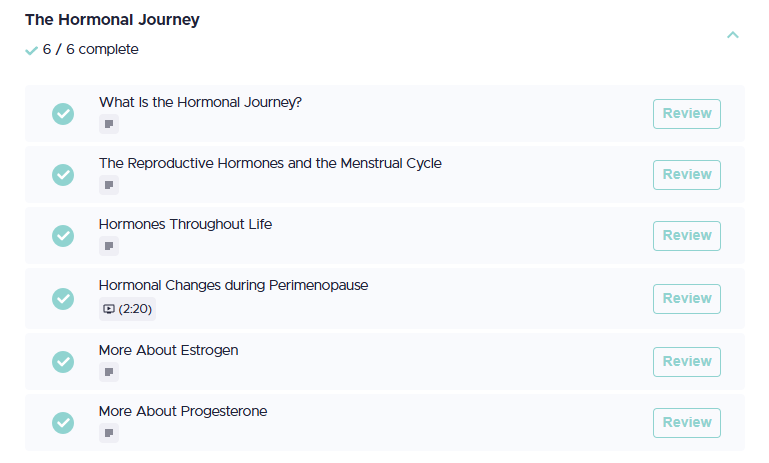
Lesson 2 - The Hormonal Journey
We need to understand the basics. If we have good foundations it will help us move forward.
Button
2.
A deeper dive into what progesterone and estrogen too so we can navigate through what you are feeling. Or prepare for changes if you don't have any symptoms.
Button
Lesson 4 - Improve Your Hormonal Wellbeing
Write your caption hereButton
Lesson 5 - When to see a doctor
Write your caption hereButton
Lesson 6 - Before Your Appointment
Write your caption hereButton
Lesson 7 - In your Appointment
Write your caption hereButton
Lesson 8 - After your Appointment
What happens if you have more questions?
Button
Ways to move forward
Write your caption hereButton