Antidepressants in PMS/PMDD
SSRIs (Selective Serotonin Reuptake Inhibitors) are medications that increase serotonin levels in the brain, helping to regulate mood and emotional responses. They are commonly used to treat depression, anxiety, and PMDD
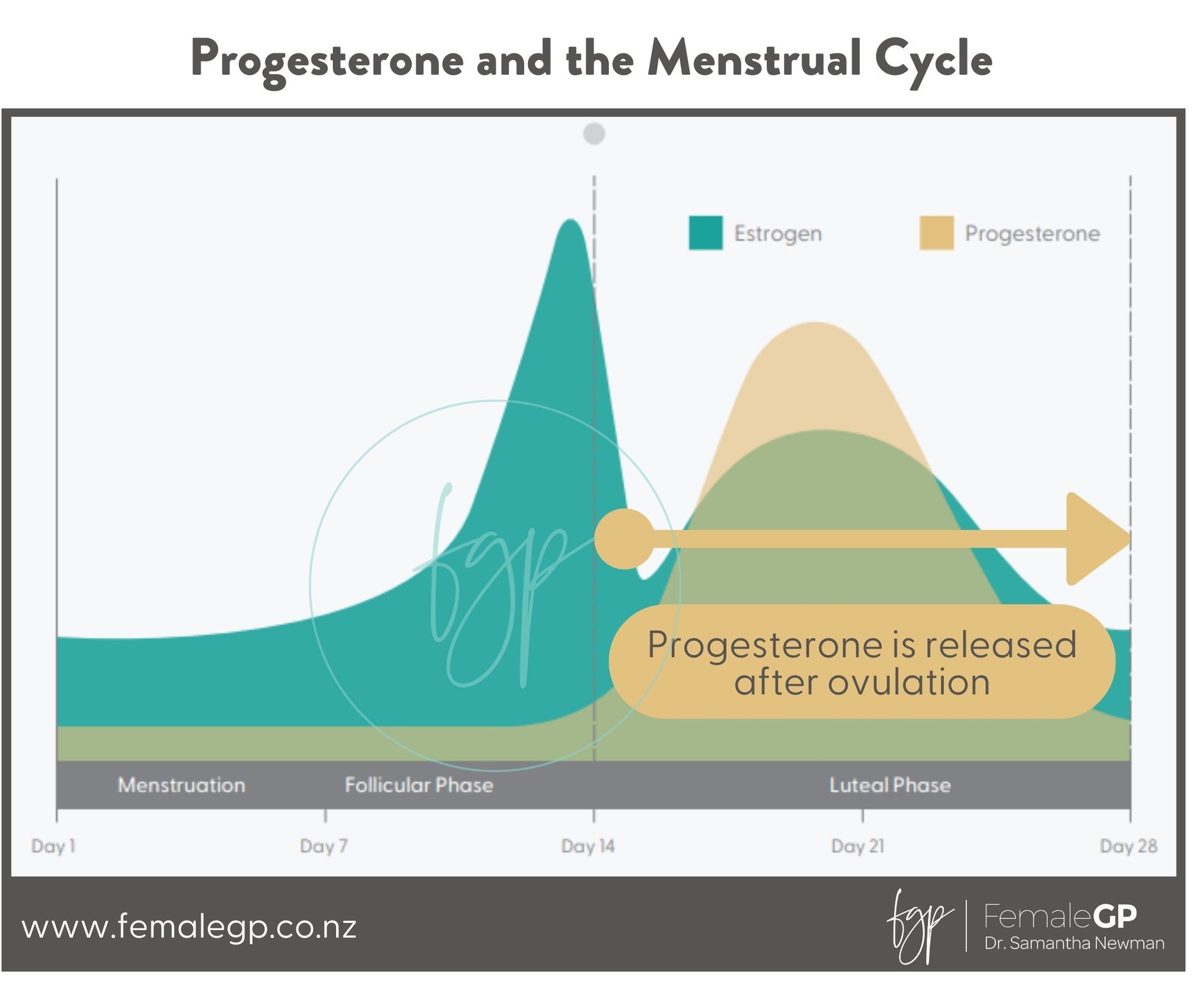
SSRIs work for PMDD by increasing serotonin availability, which helps regulate mood and emotional responses. PMDD isn’t caused by a constant serotonin deficiency like depression but by heightened sensitivity to normal hormonal fluctuations, particularly changes in progesterone and its metabolite, allopregnanolone. These fluctuations can disrupt the brain’s serotonin system, leading to mood disturbances, irritability, and other symptoms.
SSRIs help by:
• Stabilizing mood and reducing anxiety by increasing serotonin levels.
• Working rapidly, sometimes within days, likely due to their interaction with allopregnanolone .
• Easing physical symptoms, such as bloating, fatigue, and pain (higher doses may be needed).
Their effectiveness in both continuous use (daily) and luteal-phase use (only in the two weeks before menstruation) supports the idea that PMDD is a biochemical reaction to hormonal shifts—not a primary mood disorder like depression.
Studies suggest that SSRIs improve cognitive symptoms in PMDD, particularly related to emotional regulation, attention, and working memory.
Research indicates:
• Improved emotional processing – SSRIs reduce negative emotional bias, making individuals less reactive to mood swings and irritability.
• Better cognitive flexibility – They help with shifting attention and adapting to tasks, which can be impaired during the luteal phase.
• Enhanced working memory – Some studies show improvements in memory tasks, suggesting reduced mental fog and better concentration.
• Faster response times – Women with PMDD often experience slowed cognitive processing in the luteal phase, which SSRIs can help normalize.
These findings support the idea that PMDD involves temporary disruptions in brain function due to hormonal sensitivity, rather than a constant cognitive deficit.
However, as with other uses of SSRIs, there are potential side effects to be aware of. However, when using SSRIs for PMDD in a cyclical manner - the key is the lower dose. This means that side effects are much less frequent. And interestingly, there are often no adjustment onto and when stopping the medication.
Some side effects from SSRIs can include:
- Gastrointestinal disturbances – nausea, diarrhea, or stomach upset, which may be more noticeable at the start of treatment.
- Sleep issues – insomnia or excessive sleepiness, which can affect daily functioning.
- Sexual dysfunction – reduced libido, difficulty achieving orgasm, or erectile dysfunction, which can be challenging for some patients.
- Emotional blunting – some individuals report feeling "numb" or emotionally distant, which can be particularly concerning for those already experiencing emotional dysregulation with PMDD.
- Weight changes – some individuals may experience weight gain or loss.
- Increased anxiety – at the start of treatment, anxiety may worsen before improving.
- Dizziness or fatigue – can impact daily activities or worsen feelings of tiredness.
- Headaches – which can overlap with PMDD-related headaches or migraines.
What does it mean by cyclical antidepressant use?
When we prescribe cyclical SSRI use, it means taking the medication only d uring the luteal phase —the latter part of your menstrual cycle. This starts after ovulation, when progesterone begins to rise, or as soon as symptoms appear. Unlike daily SSRI use, this approach targets premenstrual symptoms without needing to take the medication every day of the month.