MEDICATION: Mirena
Perimenopause and the Mirena - is it for me?
Here's a summary of why a Mirena IUD can be beneficial during perimenopause:
- Manages heavy bleeding: It significantly reduces menstrual flow, which is often heavier and irregular during perimenopause. We recommend inserting the Mirena at the end of your period when the lining is the thinnest. The progestin release builds up the thinning effect on the uterine lining over the first 3-6 months, therefore if you have heavy periods (eg clots, flooding) this increases the rates of the Mirena being expelled so we often suggest continuing to use other progestogens or antiinflammatories in the initial stages
- Effective contraception: Provides highly reliable birth control, important as pregnancy is still possible during this transition.
- Hormone balance: Helps stabilize hormonal fluctuations common in perimenopause, potentially easing symptoms like mood swings and cramps.
- Endometrial protection: For women using estrogen therapy, it protects the uterine lining from hyperplasia. For individuals in bigger bodies, the adipose [fat] cells increase estrone [a not so nice form of estrogen] which stimulates the endometrial lining and increases rates of endometrial cancer and abnormal menstrual bleeding. The Mirena significantly decreases rates of pre cancerous and cancerous change
- Localized hormone delivery: Minimal systemic absorption means fewer side effects compared to oral medications.
- Convenience: "Fit and forget" method that lasts 5-7 years, reducing the need for daily pills.
- Versatility: Can be used as part of hormone replacement therapy (HRT) or on its own for symptom management.
- Beneficial for conditions like endometriosis and menstrual migraines.
- Minimal impact on breast health compared to some other hormonal treatments.
- Can be used alongside other treatments if needed, such as Utrogestan for sleep benefits (off licence)
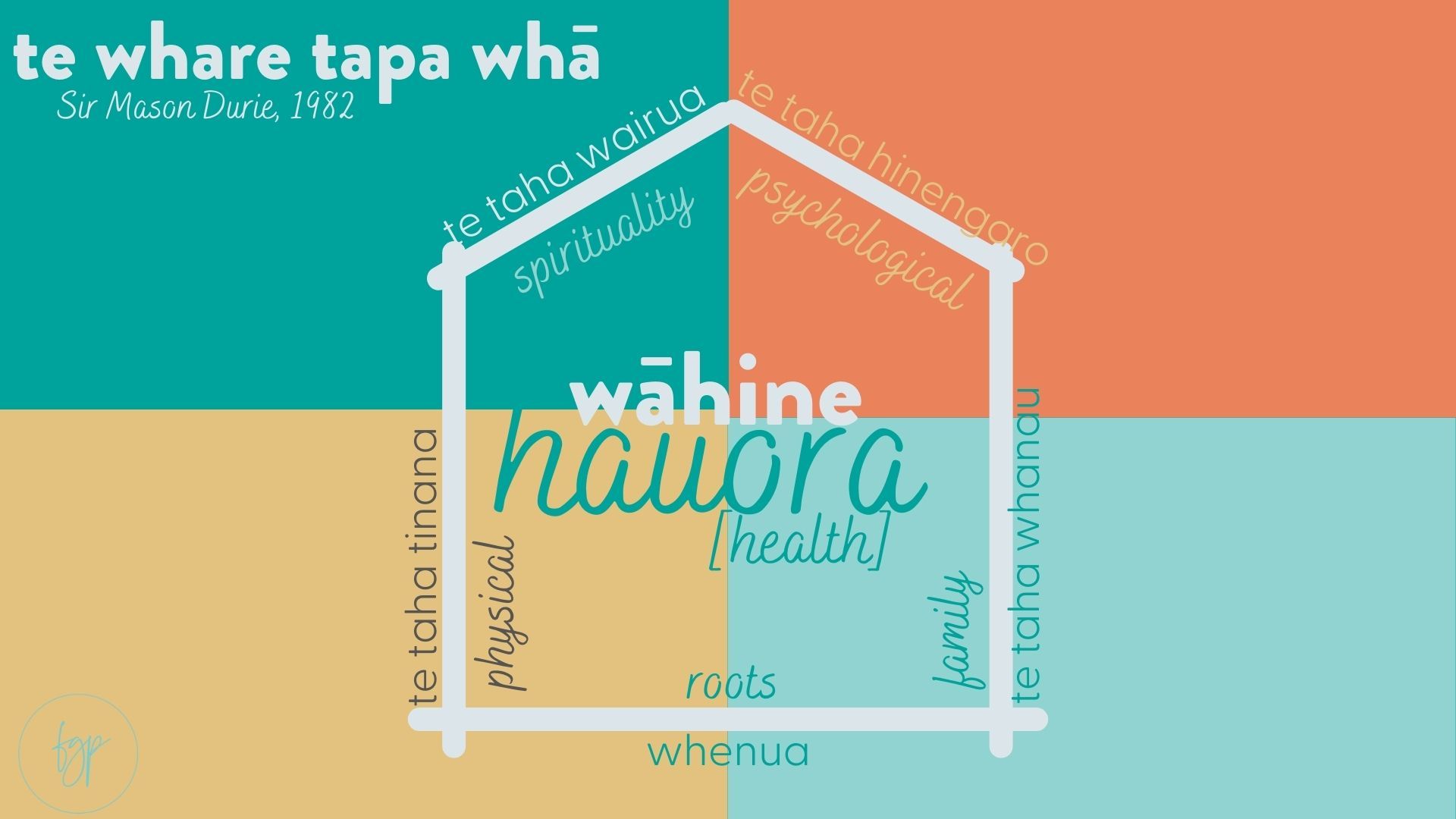
Our wellbeing and health needs evolve as we journey through life, and for many women, midlife brings new challenges, particularly when it comes to menstrual health. Heavy bleeding becomes more common during this time, and what you may have managed earlier in life can become increasingly difficult to cope with, especially when combined with other midlife factors like career demands, family responsibilities, and hormonal changes. This is where considering options like the Mirena IUS can be particularly beneficial. Not only does it provide effective contraception, but it can significantly reduce heavy menstrual bleeding, often leading to lighter periods or even no periods at all. This can be a game-changer for your quality of life, energy levels, and overall wellbeing. Moreover, with rates of hysterectomy (removal of the womb) being higher due to abnormal bleeding, exploring less invasive options like Mirena first can be a wise choice for women who wish to avoid surgery.
Remember, what worked for you in the past may not be the best solution now, and it's okay to reassess and consider new options as your body and life circumstances change.